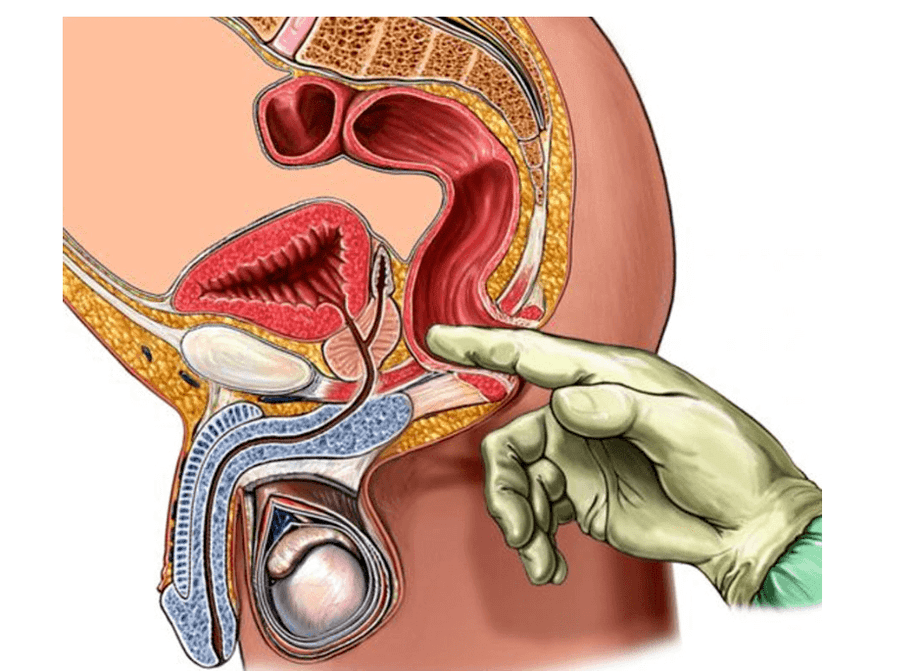
Prostatitis is an inflammatory process located in the prostate gland.This pathology is common and is usually diagnosed in men of childbearing age.The prostate (the second name for the prostate) is located beneath the bladder and partially surrounds the urethra (urethra).Therefore, even minor dysfunction of this organ can lead to genitourinary dysfunction.
Causes of prostatitis
Prostatitis is classified as an inflammatory process, but this does not mean that it is caused entirely by pathogenic microorganisms.Doctors (andrologists who treat diseases of the male reproductive system) identify several reasons for the development of related pathologies:
- Stagnation of blood in the pelvis.This refers to the disruption of blood microcirculation in the prostate and nearby organs, causing organ enlargement.Violations may occur due to a sedentary lifestyle, obesity (not necessarily severe), or during the postoperative period.
- Urogenital infections.Most often, when examining patients with prostatitis, doctors isolate gonococci, staphylococci, chlamydia and trichomonas.In rare cases, the infection penetrates the prostate against the background of a sore throat or flu - in this case, the inflammatory process in question is distinguished as a complication.
- Pelvic organs are often injured.As a result, drivers develop prostatitis - their perineum is constantly under pressure, and the prostate experiences shaking and vibrations.
- Bacteria enter through the body's biological fluids.Everyone has bacterial colonies in their intestines and urinary tract.Under normal circumstances, they are absolutely harmless, only under favorable conditions (weakened immunity, long-term medication, chronic illness, human immunodeficiency virus) they can become pathogenic and cause inflammatory processes.These bacteria can enter the prostate through the blood or lymph fluid.
In addition, when diagnosing the inflammatory process of the prostate, factors triggering the pathology can be considered:
- Frequent hypothermia - this may be due to peculiar working conditions or neglect of dress code rules for certain times of the year;
- Endocrine system dysfunction - excessive or insufficient production of male hormones, diagnosis of diabetes;
- Overly active sexual life, as well as long-term abstinence - the prostate is depleted;
- Any chronic disease - there are officially documented cases of prostatitis occurring in the context of untreated bronchitis, dental caries, cystitis and urinary tract infections.
symptoms of inflammatory process
Andrologists distinguish between primary and indirect signs of the inflammatory process of the prostate.The main symptoms appear clearly:
- Urination becomes more frequent regardless of how much fluid is consumed;
- It hurts the moment the urine comes out, and there is pain and burning in the urethra;
- The body temperature increases (congestion) to critical levels.
These symptoms are soon followed by a burning sensation throughout the perineum and pain during bowel movements.
Indirect signs of the inflammatory process of the prostate are not so obvious, but men should not ignore them:
- Ejaculation becomes too rapid - sexual intercourse takes less time;
- Nocturnal erections may be prolonged;
- Decreased libido - partial or complete;
- "Flakes" or white "threads" appear in urine.
Please note: these indirect signs indicate that the associated inflammatory process has begun to develop - it is highly treatable and does not present complications.
Prostatitis is divided into acute and chronic types, each with its own symptoms.
acute prostatitis
Acute prostatitis always starts suddenly and manifests itself in:
- temperature rise;
- Prolonged pain in the perineum;
- Frequent need to go to the toilet;
- When the bladder feels full, very small amounts of urine are passed out.
Please note: The most dangerous condition in acute inflammation of the prostate is urinary retention.In this condition, men experience a strong desire to go to the toilet but are unable to urinate even if they try hard.Acute urinary retention is accompanied by severe pain and pressure in the area of the anatomical location of the bladder—patients describe their condition as "bladder about to burst."This condition requires immediate medical attention, including the use of a catheter - which is inserted into the urethra and bladder to literally "push" away the swollen glands.When the catheter reaches the bladder, urine begins to flow out, the patient feels immediate relief and the condition returns to normal within a short period of time.
chronic prostatitis
This type of pathology is virtually asymptomatic - occasionally, men experience short-term pain in the perineum (similar to low back pain), notice changes in sexual intercourse - it can be lengthened or shortened.In addition, patients may become irritable and have restless sleep at night, their urine flow may become weak (due to narrowing of the urethra), and flakes or lines of white clots may appear in their urine in the morning.
Please note: Chronic forms of the prostatic inflammatory process may occur without the patient noticing.The fact is that in youth, the symptoms of acute prostatitis are mild, and if a young man drinks too much or is too enthusiastic about his work, then he has no time to pay attention to changes in urination or cyclic pain in the perineum.The symptoms of acute prostatitis disappear over time, but that doesn't mean the disease has subsided—it's just become chronic.
Treatment methods for prostatitis
Treatment of inflammatory processes of the prostate can only be carried out under the supervision of an andrologist.He not only diagnoses prostatitis itself (which often has the same symptoms as prostate cancer), but also reveals the real reasons why it occurs.Generally speaking, several different treatments are available to treat prostate inflammation.
drug treatment
For prostatitis, antibacterial agents (antibiotics) can be prescribed, but only if the pathogenic bacteria are isolated during the examination and confirmed to be the cause of the development of the pathology.In addition to antibiotics, patients need to take probiotics or prebiotics - these drugs normalize the intestinal flora and combat the development of pathological processes in the intestine.
If the inflammatory process begins due to the negative influence of external factors (hypothermia, injury), you need to take nonsteroidal anti-inflammatory drugs.
If a hormonal imbalance occurs, men must undergo a course of hormonal therapy.
Please note: Medications vary greatly and must be chosen on an individual basis - self-medication is strictly prohibited in this case.
physical therapy
Treatment of prostatic inflammation should be comprehensive.In the context of the use of drugs, it will be effective to perform certain physical procedures:
- Electrical stimulation speeds up metabolic processes, triggers more active hormone production, and restores glandular structure.
- Magnet therapy is a painless procedure that helps reduce inflammation levels and eliminate prostate swelling.
- Prostate Massage - Performed only after treatment of acute inflammation; the procedure is painful but very effective.
traditional medicine
Please note: Recipes from the traditional medicine category should not be the only method of treatment - they can only speed up the healing process and enhance the effectiveness of medication and physical therapy.
The most effective and safe traditional treatments include:
- Eat pumpkin seeds.They contain zinc, an essential element for male health, so for prostatitis, throughout the treatment, you need to eat 30 raw seeds 30 minutes before meals.
- Pumpkin Honey Balls.Peel 100 grams of raw pumpkin seeds, grind them with a meat grinder (or blender, but do not grind them into fine particles), and mix with 200 grams of honey.Roll the resulting mass into small balls and store them in the refrigerator.You need to eat 1-2 pellets before eating (30 minutes before) - no need to chew, it is best to dissolve slowly.Continue this treatment until the symptoms of prostatitis disappear.
- Hazel leaf soup.You can gather hazel leaves yourself or purchase the dry ingredients at a drug store; there is a cup of boiling water for each tablespoon of ingredients.The decoction is brewed for 20 minutes like ordinary tea, filtered and taken in 50 ml, at least 4 times a day.Please note: Hazel bark is also sold in pharmacies - it can also be used to treat prostatitis, and with the same prescription.But remember, for bark, the brewing time will be doubled.
- Parsley juice.Made from the green leaves of the plant, take 1 dessert spoon 3 times daily before meals.
- Parsley seed soup.You need to take 1 tablespoon of parsley seeds, pour 400 ml of boiling water and leave for 2 hours (you can do this in a thermos).Take 1 tablespoon of decoction in the morning and evening every day.
Regardless, no matter how safe the treatment appears to be, you should always consult your doctor first.For example, if a man suffers from gallstones in addition to prostatitis, then he is strictly prohibited from using pumpkin seeds - any prescription is strictly based on individual circumstances.
diet and lifestyle
To get the best results during prostatitis treatment, you need to stick to a certain diet.It should exclude fatty meats, smoked and too salty foods, baked goods and chocolate from the diet.The menu includes fish and seafood, milk and its derivatives, steamed vegetables.Drinking fresh vegetable and fruit juices is very useful in treating prostatitis - they will help strengthen and restore the immune system.
During treatment, you will need to abstain from alcohol and lead an active lifestyle - at least doing morning exercises, walking more and losing excess weight.
Prostatitis is not considered a life-threatening disease in men, but ignoring its symptoms can lead to serious complications.One of the most serious consequences is male infertility and loss of erectile function, which often occurs with long-term chronic prostatitis.























